Adenomyosis: A Comprehensive Overview
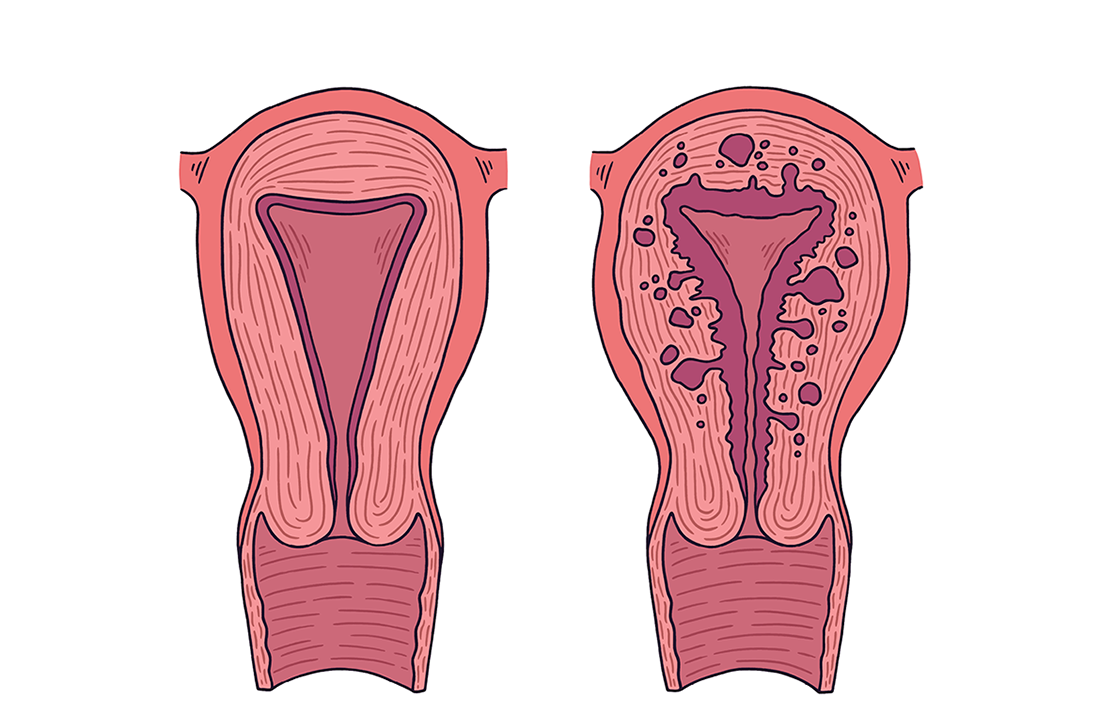
Adenomyosis is a benign gynecological condition where the tissue that normally lines the uterus (the endometrium) grows into the muscular wall of the uterus (the myometrium). This misplaced tissue still acts like a normal endometrium, thickening and bleeding during the menstrual cycle, which can cause the uterus to become enlarged.
Incidence in World and India
It’s hard to know the exact number of adenomyosis cases because diagnosis is tricky and often requires a hysterectomy for confirmation. However, studies show a wide range of prevalence, from 5% to 70% in hysterectomy specimens worldwide. The condition is most common in women aged 35 to 50, but it is being diagnosed more often in younger women and even adolescents.
In India, prevalence rates also vary greatly, from 6% to 55% in studies based on hysterectomy specimens. Despite these challenges, adenomyosis is a major health concern, with some estimates suggesting it affects around 42 million women in India. It is a frequent cause of abnormal uterine bleeding and pelvic pain, often leading to hysterectomy.
Symptoms
The symptoms of adenomyosis can vary widely among individuals, with some women experiencing no symptoms at all, while others suffer from debilitating pain and heavy bleeding. The severity of symptoms often correlates with the extent of endometrial tissue invasion into the myometrium. Common symptoms include:
- Heavy or Prolonged Menstrual Bleeding (Menorrhagia)
- Severe Menstrual Cramps (Dysmenorrhea)
- Chronic Pelvic Pain
- Abdominal Pressure and Bloating
- Painful Intercourse (Dyspareunia)
- Painful Bowel Movements or Urination
- Enlarged Uterus
- Bleeding Between Periods
It’s important to note that these symptoms can also be indicative of other gynecological conditions, making accurate diagnosis crucial.
Diagnosis
Diagnosing adenomyosis can be challenging because its symptoms often overlap with other gynecological conditions, such as uterine fibroids and endometriosis. Historically, a definitive diagnosis of adenomyosis could only be made through histopathological examination of the uterus after a hysterectomy. However, advancements in imaging techniques have made it possible to diagnose adenomyosis non-invasively.
Diagnostic Methods:
1.Clinical Suspicion and Pelvic Examination: The diagnostic process usually begins with a thorough medical history and a pelvic examination. During the examination, a healthcare provider may notice an enlarged, boggy, or tender uterus, which can raise suspicion for adenomyosis.
2.Transvaginal Ultrasonography (TVS): TVS is often the first-line imaging modality used to evaluate the uterus. While it can be challenging to definitively diagnose adenomyosis with ultrasound alone, certain features are highly suggestive of the condition, including:
- Heterogeneous myometrial echotexture: The uterine muscle may appear irregular or mottled.
- Myometrial cysts: Small, fluid-filled pockets within the uterine wall.
- Asymmetrical thickening of the myometrium: One wall of the uterus may be thicker than the other.
- Subendometrial striations or linear shadowing: Bright lines or shadows extending from the endometrium into the myometrium.
- Poorly defined endometrial-myometrial junction: The boundary between the lining and the muscle may be indistinct.
3.Magnetic Resonance Imaging (MRI): MRI is considered the most accurate non-invasive imaging technique for diagnosing adenomyosis. It provides detailed images of the uterus and can clearly delineate the endometrial-myometrial junction. Key MRI findings indicative of adenomyosis include:
- Junctional Zone (JZ) thickening: The JZ, a distinct inner layer of the myometrium, appears thickened (typically >12 mm).
- High-intensity foci: Bright spots within the myometrium on T2-weighted images, representing ectopic endometrial glands or small cysts.
- Linear striations: Radial lines extending from the endometrium into the myometrium.
4.Endometrial Biopsy: While an endometrial biopsy can rule out other conditions, such as endometrial cancer, it is generally not effective for diagnosing adenomyosis because it only samples the uterine lining and not the muscle wall.
5.Hysteroscopy and Laparoscopy: These invasive procedures are typically not used for primary diagnosis of adenomyosis. However, they may be performed to rule out other conditions or to assess the extent of adenomyosis if other imaging methods are inconclusive. Direct visualization during laparoscopy may reveal an enlarged, globular uterus, but definitive diagnosis still relies on histopathology.
It is crucial for healthcare providers to integrate clinical findings with imaging results to make an accurate diagnosis and differentiate adenomyosis from other conditions with similar symptoms.
Cause and Aetiology
The exact cause of adenomyosis is not fully understood, and several theories have been proposed to explain its development. It is likely a multifactorial condition, with a combination of genetic, hormonal, and environmental factors contributing to its onset. The primary characteristic of adenomyosis is the abnormal growth of endometrial tissue into the myometrium, and the leading theories attempt to explain how this invasion occurs.
Theories of Aetiology:
1.Invasive Tissue Growth Theory: This is the most widely accepted theory. It suggests that endometrial cells from the lining of the uterus directly invade the underlying muscular wall. This invasion might occur due to a breach in the endometrial-myometrial junction, a natural boundary between the two layers. Factors that could contribute to this breach include:
- Uterine Trauma: Procedures such as uterine surgery (e.g., C-sections, myomectomies, or dilation and curettage procedures) are thought to potentially damage the endometrial-myometrial junction, allowing endometrial tissue to infiltrate the myometrium.
- Inflammation: Chronic inflammation within the uterus might also disrupt the integrity of the endometrial-myometrial junction, facilitating the invasion of endometrial cells.
2.Developmental Origin Theory: This theory proposes that adenomyosis originates from misplaced embryonic müllerian tissue that is incorporated into the myometrium during uterine development. These embryonic cells could then develop into endometrial tissue within the muscle wall later in life.
3.Stem Cell Theory: This theory suggests that stem cells within the myometrium or endometrium may play a role in the development of adenomyosis. These stem cells could have the ability to differentiate into endometrial tissue within the myometrium.
Risk Factors:
While the exact cause remains elusive, several factors are associated with an increased risk of developing adenomyosis:
- Age: Adenomyosis is most commonly diagnosed in women in their late reproductive years, typically between 35 and 50 years old. This suggests a possible link to prolonged exposure to estrogen.
- Parity: Women who have had children are more likely to develop adenomyosis. The stretching and contraction of the uterus during pregnancy and childbirth may contribute to the invasion of endometrial tissue into the myometrium.
- Prior Uterine Surgery: As mentioned, a history of uterine surgery, particularly C-sections, is a recognized risk factor.
- Hormonal Influences: Estrogen is believed to play a significant role in the development and progression of adenomyosis. The ectopic endometrial tissue in the myometrium is responsive to hormonal fluctuations, particularly estrogen, which promotes its growth and activity. Progesterone and prolactin have also been implicated in some studies.
- Genetic Predisposition: While not fully established, there may be a genetic component to adenomyosis, as it sometimes runs in families.
It’s important to distinguish adenomyosis from endometriosis. While both involve endometrial-like tissue, endometriosis involves this tissue growing outside the uterus, whereas adenomyosis is confined to the uterine muscle wall. However, the two conditions can coexist, and they share some common symptoms and potential underlying mechanisms.
Medical Management
Medical management of adenomyosis primarily focuses on alleviating symptoms, particularly heavy menstrual bleeding and pain, as there is no cure for the condition other than hysterectomy. The choice of medical treatment depends on the severity of symptoms, the patient’s age, desire for future fertility, and overall health. Medical therapies aim to suppress the growth and activity of the ectopic endometrial tissue by targeting hormonal pathways.
Common Medical Treatments:
1.Nonsteroidal Anti-inflammatory Drugs (NSAIDs): For mild to moderate pain, NSAIDs such as ibuprofen or naproxen can be used to reduce menstrual cramps. They are most effective when started a day or two before the period and continued throughout menstruation.
2.Hormonal Therapies: These are the cornerstone of medical management for adenomyosis, aiming to reduce estrogen levels or create a hormonal environment that suppresses endometrial tissue growth.
- Combined Oral Contraceptives (COCs): Birth control pills can help regulate menstrual cycles, reduce menstrual flow, and alleviate pain by thinning the endometrial lining and suppressing ovulation. Continuous use of COCs can also be an option to minimize periods.
- Progestin-Only Therapies: Progestins can be administered in various forms:
- Levonorgestrel-Releasing Intrauterine System (LNG-IUS): This device releases a small, steady dose of levonorgestrel directly into the uterus. It is highly effective in reducing heavy menstrual bleeding and pain by thinning the endometrial lining and suppressing its growth. It can provide long-term relief for several years.
- Oral Progestins: Medications like dienogest or medroxyprogesterone acetate can be taken orally to suppress endometrial growth and reduce bleeding and pain.
- Progestin Injections or Implants: These provide long-acting hormonal contraception and can also help manage adenomyosis symptoms.
- Gonadotropin-Releasing Hormone (GnRH) Agonists: These medications (e.g., leuprolide) induce a temporary, reversible menopause-like state by suppressing estrogen production from the ovaries. This leads to a significant reduction in menstrual bleeding and pain. However, due to potential side effects like hot flashes, bone density loss, and mood changes, their long-term use is limited, often to 3-6 months. Add-back therapy (low-dose estrogen and progestin) can be used to mitigate these side effects.
- GnRH Antagonists: Newer oral medications (e.g., elagolix, relugolix) that also suppress estrogen production but offer a more rapid onset of action and can be used for longer durations with appropriate add-back therapy.
3.Tranexamic Acid: This non-hormonal medication helps reduce heavy menstrual bleeding by promoting blood clotting. It is taken only during menstruation.
Other Considerations:
- Pain Management: Beyond NSAIDs, other pain relief strategies, including physical therapy, acupuncture, or nerve blocks, may be considered for chronic pelvic pain.
- Iron Supplementation: For women experiencing heavy bleeding and iron-deficiency anemia, iron supplements are crucial to restore iron levels.
Medical management is often the first-line approach, especially for women who wish to preserve their fertility or avoid surgery. While these treatments can effectively manage symptoms, they do not eliminate the adenomyosis itself. Symptoms may recur once medical therapy is discontinued.
Surgical Management
Surgical management of adenomyosis is considered when medical therapies fail to control symptoms, or when symptoms are severe and significantly impact a woman’s quality of life. The choice of surgical approach depends on the patient’s desire for future fertility and the extent of the disease.
- Hysterectomy:
Hysterectomy, the surgical removal of the uterus, is the only definitive cure for adenomyosis. Since adenomyosis involves the invasion of endometrial tissue into the uterine muscle, removing the entire uterus eliminates the source of the problem. This option is typically considered for women who have completed childbearing, have severe and debilitating symptoms, and have not responded to conservative medical or surgical treatments. While effective, hysterectomy is a major surgical procedure with associated risks and recovery time.
- Conservative Surgical Approaches (Uterus-Sparing Surgery):
For women who wish to preserve their fertility or avoid hysterectomy, conservative surgical options aim to remove or reduce the adenomyotic tissue while preserving the uterus. These procedures are often more challenging due to the diffuse nature of adenomyosis within the uterine wall, making complete excision difficult.
- Adenomyomectomy: This procedure involves surgically excising the adenomyotic lesions from the uterine muscle. It is similar to a myomectomy (removal of fibroids) but is more complex due to the ill-defined borders of adenomyotic tissue. Adenomyomectomy can be performed via laparotomy (open surgery) or laparoscopy (minimally invasive surgery). While it can significantly reduce symptoms and improve fertility outcomes in some cases, there is a risk of recurrence of adenomyosis and potential complications such as uterine rupture during subsequent pregnancies.
- Uterine Artery Embolization (UAE): Although primarily used for uterine fibroids, UAE can also be considered for adenomyosis. This procedure involves blocking the blood supply to the uterus, which can lead to a reduction in uterine size and symptom relief. It is a less invasive option but may not be as effective as hysterectomy or adenomyomectomy for severe adenomyosis.
- Endometrial Ablation: This procedure involves destroying the lining of the uterus to reduce heavy bleeding. While it can be effective for menorrhagia, it is generally not recommended as a primary treatment for adenomyosis, especially if pain is a prominent symptom, as it does not address the adenomyotic tissue within the myometrium. It is also not suitable for women desiring future fertility.
Considerations for Surgical Management:
- Fertility Preservation: For women who desire future pregnancies, conservative surgical options are explored, but they carry risks and may not guarantee complete symptom resolution or successful pregnancy.
- Symptom Severity: The decision for surgery is often driven by the severity of symptoms and their impact on daily life.
- Patient Preference: A thorough discussion between the patient and healthcare provider is essential to weigh the benefits and risks of each surgical option and align with the patient’s goals and preferences.
It is important to note that while conservative surgeries can offer symptom relief and fertility preservation, adenomyosis can recur, and some women may eventually require a hysterectomy if symptoms persist or worsen.

