BEST ENDOMETRIOSIS SPECIALIST FOR TREATMENT
WELCOME TO MY GARDEN
WELCOME TO MY GARDEN
Member of European Endometriosis League
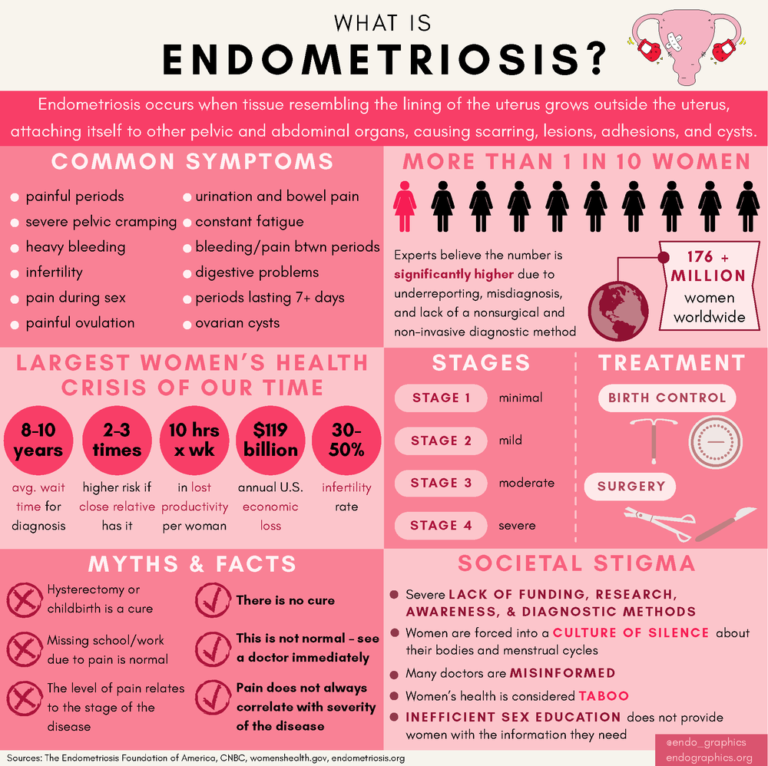
- 1 in 10 Women experience endometriosis in their reproductive years between ages (15 and 49).
- 20-25 % of women with endometriosis have no symptoms.
- 30-35 % of women with endometriosis are infertile.
- 7.5 years the average it takes from the onset of symptoms until proper diagnosis.
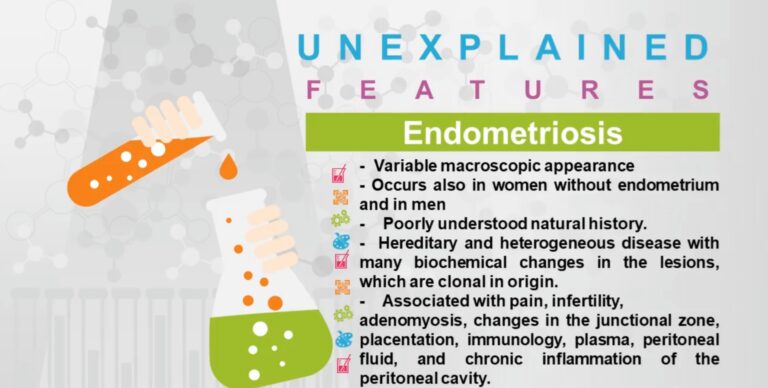
It is a condition that occurs when tissue similar to the inside lining of the uterus is found outside of its normal location. Endometrial implants can be found on the ovaries, fallopian tubes, and ligaments that support the uterus and tissue covering the bladder and rectum. The most common locations of endometrial implants in teens are in the cul–de–sac area (behind the uterus), and near the bladder.
Live Television discussion With Dr GSS Mohapatra about Endometrosis
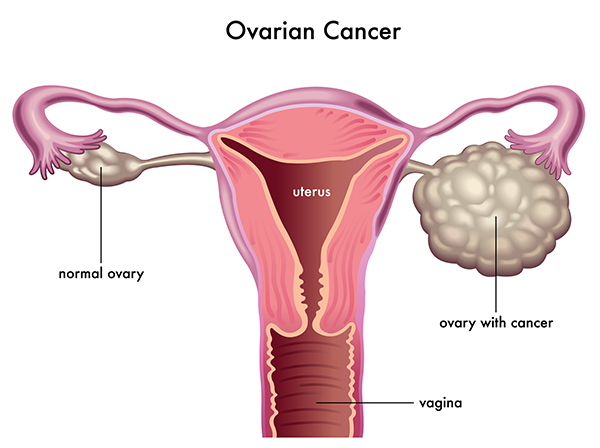
The exact cause is not known. It is thought that some cells from the womb (uterus) lining (the endometrium) get outside the uterus through the tubes by retrograde flow into the pelvic area. The ‘spilt’ endometrial cells then continue to survive next to the uterus, ovary, bladder, bowel, or Fallopian tube or even on previous scars like that of caesarean section. The cells respond to the female hormone oestrogen, just like the lining of the uterus does each month. Throughout each month the cells multiply and swell, and then break down as if ready to be shed at the time of your period. However, because they are trapped inside the pelvic area, they cannot escape. They form patches of tissue called endometriosis. Patches of endometriosis tend to be adhesion forming and may hence join organs to each otherlike bowel to the uterus, omentum to the uterus, ovaries and uterus etc.The cysts can fill with dark blood; this is known as ‘chocolate cysts’.
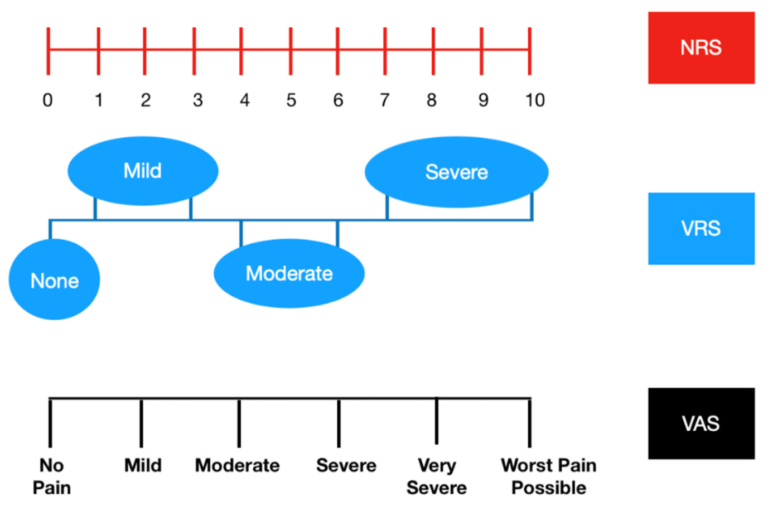
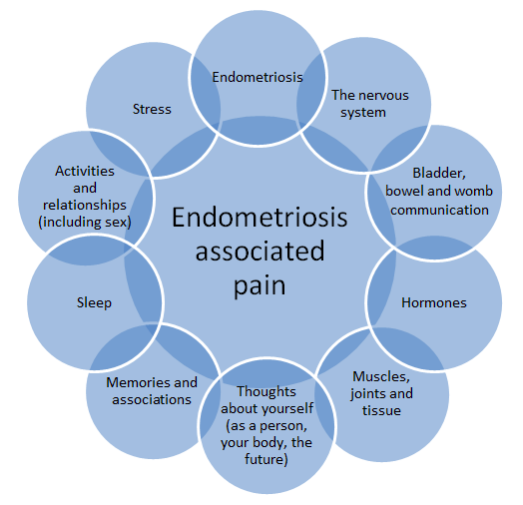
With each menstrual cycle, the implants go through the same growing, breaking down, and bleeding that the uterine lining (endometrium) goes through. This is why endometriosis pain may start as mild discomfort a few days before the menstrual period and then usually is gone by the time the period ends. But if an implant grows in a sensitive area, it can cause constant pain or pain during certain activities, such as sex, exercise, or bowel movements.
Between 20% and 40% of women who are infertile have endometriosis.
Pain is the main symptom of endometriosis. You may have:
- Painful periods
- Pain prior to and after menses
- Pain during or following sexual intercourse
- Pain with bowel movements
- Transvaginal ultrasound
- Pelvic laparoscopy
- Painful periods
- Pain prior to and after menses:dysmenorrhoea
- Pain during or following sexual intercourse:dyspareunia
- Pain with bowel movements:dyschezia
- Pain during micturition: dysuria
- Bleeding during urination:haematuria
- Infertility (the inability to become pregnant) or subfertility (a reduced ability to become pregnant)
- Pelvic pain: in women with endometriosis depends partly on where endometrial implants of endometriosis are located.
- Deeper implants and implants in areas of high nerve density are more apt to produce pain.
- The implants may also release substances into the bloodstream, which are capable of eliciting pain.
- Pain can result when endometriotic implants incite scarring of surrounding tissues. There appears to be no relationship between severity of pain and the amount of anatomical disease which is present.
Transvaginal ultrasound:An ultrasound may not be able to detect subtle changes due to endometriosis but can help to diagnose an endometrioma/chocolate cyst of any size.A transvaginal ultrasound can detect whether every organ in the pelvis has become adherent to each other( VISCERAL SLIDING SIGN).It can also detect rectovaginal nodule and the size of the nodule in the vagina, how much of the rectum is involved, only if the sonologist doing the scan is skilled enough.
MRI: MRI is the second-line imaging technique after USG. Deep pelvic endometriosis causes chronic pelvic pain and infertility. MRI is one the best imaging technique for preoperative staging of endometriosis.
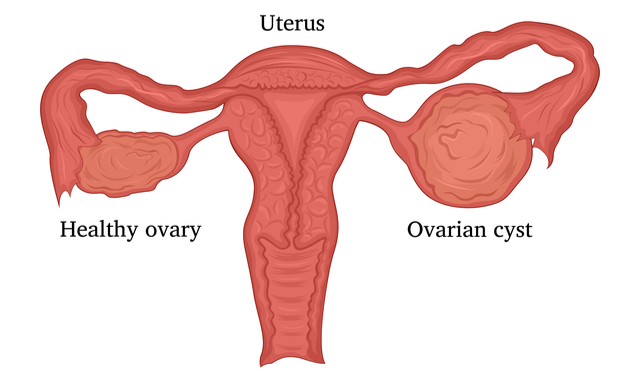
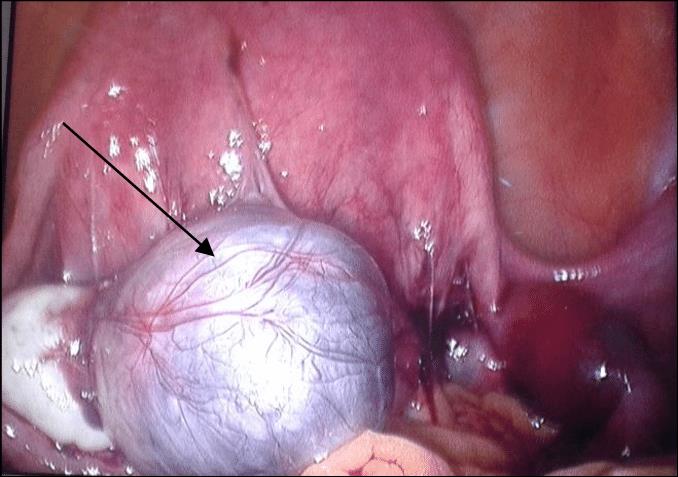
A chocolate cyst is a type of ovarian cyst filled with old altered blood. These cysts, which gynaecologists call endometriomas, are not usually cancerous, though they usually mean that a person’s endometriosis is severe enough to complicate their fertility. Between 20 and 40 percent of people with endometriosis develop chocolate cysts. They get their name from their brown, tar-like appearance, looking something like melted chocolate. They’re also called ovarian endometriomas.
The colour comes from old menstrual blood and tissue that fills the cavity of the cyst. A chocolate cyst can affect one or both ovaries, and may occur in multiples or singularly.When occurs in both the ovaries, they often get adherent to the posterior surface of the uterus and close to each other called as KISSING OVARIES.
How can endometriosis be diagnosed?
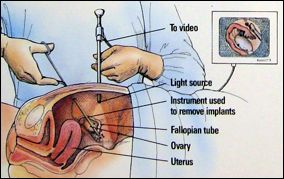
There are a number of diagnostic tools that physicians use that may raise suspicion of endometriosis, but the only definitive method of diagnosis is through minimally invasive laparoscopic surgery and biopsy of affected tissue. If you suspect you have endometriosis, ask your physician about these different diagnostic tools (see below). Don’t be afraid to get a second opinion if you feel that you need more information about endometriosis diagnosis
• At present, there is no known cure for endometriosis, and treatment is usually aimed at controlling symptoms . • Access to early diagnosis and effective treatment of endometriosis is important, but is limited in many settings, including in low- and middle-income countries- There is a need for more research and awareness raising around the world to ensure effective prevention, early diagnosis, and improved management of the disease.
How can endometriosis be diagnosed?
There are a number of diagnostic tools that physicians use that may raise suspicion of endometriosis, but the only definitive method of diagnosis is through minimally invasive laparoscopic surgery and biopsy of affected tissue. If you suspect you have endometriosis, ask your physician about these different diagnostic tools (see below). Don’t be afraid to get a second opinion if you feel that you need more information about endometriosis diagnosis.
Definitive Diagnosis
LAPAROSCOPIC SURGERY
Laparoscopic surgery is achieved by first making 2-4 small incisions on the skin of the abdomen. Through those small incisions, ports are created to the abdominal and pelvic cavities inside, which are inflated with sterile CO2 gas. The doctor will then use a tool called the laparoscope, which is a camera, through these ports to examine the tissue and organs in the abdominal and pelvic cavity
Definitive Surgery
Definitive surgery is performed when there is diffuse involvement of endometriosis to a particular site, and involves the removal of organs. The most common form of definitive endometriosis surgery is a hysterectomy (removal of the uterus). This can either include or exclude removal of the ovaries and cervix depending on the form of hysterectomy the patient and physician agree upon. As undergoing a hysterectomy is a serious decision, it is crucial that the patient and physician fully discuss the necessity for this procedure and that the patient is comfortable with their decision.
- While there are diagnostic tools used to raise suspicion of the disease or find congenital abnormalities that may be exacerbating symptoms, they cannot specifically confirm if a patient has endometriosis. Instead, these tools can be used in conjunction with diagnostic laparoscopy and an accompanying pathology report.
A physician may be able to suspect that you have endometriosis based on the information you provide during your consultation.
• It will be beneficial to explain your symptoms and pain with as much detail as possible. Bring in previous medical records, journals, symptom trackers or any materials that can provide essential information.
• Be prepared to ask questions. Visit this page to learn more about preparing yourself for an appointment
A focused pelvic exam is typically considered to be a preliminary step in the diagnosis process
• The exam will include examining the pelvis and pelvic organs and will evaluate for specific points of tenderness.
• An ultrasound may be used to gain additional information, sometimes during the same visit as the initial pelvic exam. This device is used to send sound waves to produce images of the inside of the body. It is a safe method of imaging that does not expose one to any radiation. There are two main types often used by OB/GYNs:
• Transvaginal Ultrasound: Rather than using the probe on the outside of the stomach or pelvic region, it is inserted into the vagina. This can be done during any phase of the menstrual cycle.
• Magnetic resonance imaging (MRIs) produce very detailed and clear images of tissues and organs and can be used to assist in definitive diagnosis.
-
Conservative Surgery
While there is no definitive cure for endometriosis, there are several options that have proven highly effective and have provided symptom relief for patients. Conservative surgery is an endometriosis surgery technique that is most often performed when endometriosis lesions can be well-recognized and specifically removed, leaving healthy organ tissue intact. Only the affected tissue is removed in this approach. While there are many different techniques of conservative surgery, laparoscopic excision surgery is the gold standard of treatment for endometriosis.
Deep-excision is performed during laparoscopic excision surgery, where the surgeon carefully excises or removes the entire lesion from wherever it is found, including the tissue beneath the surface. Endometriosis acts like an iceberg – despite the disease being identified above the surface of the tissue, the majority is implanted into the tissue below the surface. This is why it is so important to find a surgeon who removes lesions in their
entirety. For information about identifying a proper excision surgeon and preparing for your visit to the doctor please visit this page. It is ideal to have surgery with minimal use of heat and electricity. Often times, surgeons will use techniques such as ablation with a laser or cauterization (energy generated from electricity) to “burn off and destroy” endometriosis lesions. However, this increases the chance of not fully removing the endometriosis lesions and risks damaging the surrounding healthy tissue. This does not mean that lasers and high-energy devices cannot be used during surgery, as they can often be helpful for coagulation (stopping bleeding), but they should not be used for removing lesions themselves. Ablation or cauterization only remove the tissue on the surface but neglect the tissue growing beneath the surface. In most cases, ablation/cauterization surgery will not be effective for long-term management of endometriosis because the tissue remains below the surface. Excess scar tissue can also form using these methods due to the high energy and heat applied to surround healthy tissue. In many cases, the inflammation following ablation and cauterization can be another source of pain. We do not recommend ablation/cauterization surgery. Excision surgery is the gold standard for treatment. If a patient is considering surgery, it is important that they ask their surgeon the method for removal.
WELCOME TO MY GARDEN
Definitive Surgery
There are many ways of obtaining endometriosis relief, but it must be noted that the options below do not treat the endometriosis itself – they rather serve to alleviate some of the symptoms caused by the condition. These include:
It is a common myth that having a hysterectomy will cure endometriosis. There is no cure for endometriosis and a hysterectomy is rarely the best treatment. Most endometriosis is located in areas other than the reproductive organs. If you simply remove the uterus and do not excise the remaining lesions, patients will continue to have pain. Decisions regarding a hysterectomy should be made with a doctor experienced in treating endometriosis and should only be performed if agreed upon by the patient.
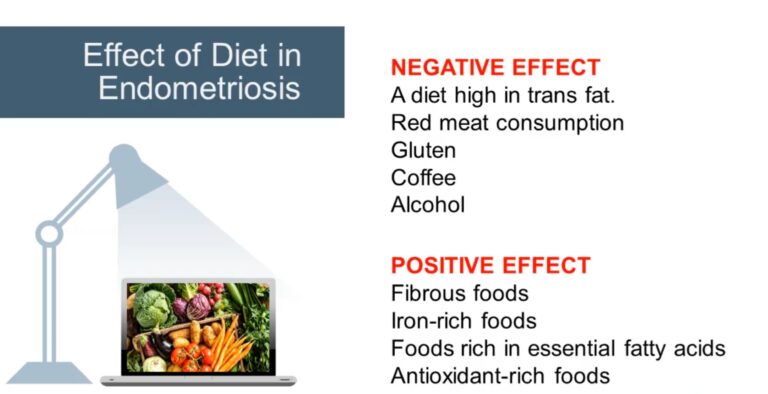
- It’s important to take good care of your body during pregnancy. We recommend you avoid alcohol, limit your caffeine intake and steer clear of any nonprescription drugs throughout your pregnancy. Indulging in alcohol can adversely affect your baby’s brain or spinal development, too much caffeine has been linked to a higher instance of miscarriage, and nonprescription drugs can lead to birth defects or behavioral problems.
While all of the above options could be helpful to relieve symptoms, every patient will benefit differently from each treatment. What may work for one person, may not for another. Endometriosis is a disease that still requires much more research. It is crucial for each patient to trust their own judgment, work with their physician, and find the pain management strategy that works best for them if they decide to explore alternative treatment measures.
As the medical community’s understanding of endometriosis is constantly growing, it is essential to choose a doctor who keeps track of these updates and is highly experienced in this condition’s diagnosis and treatment. A physician should be willing to discuss the impact of endometriosis on all aspects of a patient’s life and should share their findings in an organized, compassionate, and structured way.
Due to the limited amount of knowledge and training in endometriosis, it has a tendency to be misdiagnosed and mistreated. This is why in order to choose the right doctor, it is crucial that patients themselves are knowledgeable about the condition. Patients should ask their physician the right questions, which in the case of endometriosis all center around the patient’s period. If symptoms are worsening or synchronizing around the time of the patient’s period, this must be noted. These symptoms can include abnormally heavy or painful periods, but also painful bowel movements, diarrhea, nausea, vomiting, etc. If two or more of the symptoms do in fact coincide with a patient’s period, then a presumptive diagnosis should include endometriosis.
When patients receive a diagnosis of endometriosis, they will begin to explore their treatment options with their physician. This should ensure a thorough discussion, where the physician explains the risk and benefit of each treatment. Again, patients should draw on their own knowledge and research which they have performed to ensure their physician is providing them with the best treatment for their particular case. If at any point a patient feels uncomfortable with their physician, or loses trust in the care they receive, they should not hesitate to seek a new provider. To learn more about choosing a doctor, visit this page.
-
Expert recommendations
The occurrence of endometriosis and the impact of symptoms should not be underestimated in adolescent patients, to ensure timely diagnosis and treatment initiation • In adolescent patients, surgical diagnosis of endometriosis should be avoided in favour of clinical diagnosis based on symptoms • For adolescent patients with endometriosis, multiple treatment options are available and the use of dienogest 2 mg has been investigated in this patient population. However, treatment decisions should be made on an individual basis, using a risk–benefit approach that considers efficacy and safety.
Expert recommendations
Data support the efficacy of COCs in reducing dysmenorrhea in women with endometriosis but not the relief of other typical pain symptoms (e.g. dyspareunia, non-cyclic pelvic pain)
• COCs containing estrogen (ethinylestradiol or estradiol) and progestin components have additional contraindications and side effects compared with progestin-only products, such as dienogest16. A history of OC use for dysmenorrhea is associated with diagnosis of endometriosis, particularly of DIE, later in life.
• The rationale and evidence for OCs in the treatment of endometriosis are limited. Progestins (including dienogest) may be a better first-line treatment option with fewer contraindications compared with COCs16
• The role of dienogest 2 mg in the management of fertility requires further investigation
Management of bleeding irregularities
Treatment with dienogest 2 mg, as with other progestins, leads to endometrial regression and bleeding irregularities Initial bleeding during the first few months can be consistent,

- Long-term treatment of endometriosis with dienogest 2 mg (>15 months) should continue for as long as needed by the individual woman (e.g. until pregnancy is desired, disease recurs, or side effects occur), based on local treatment labels
- The efficacy of dienogest 2 mg should be measured primarily by its impact on pain and quality of life for the woman
- Other important considerations are effects of medical management on menstrual bleeding, reduction of lesion size, preservation of fertility, and the ability to avoid or delay surgery
- Small decreases in BMD have been seen with dienogest treatment
- Before treatment initiation, patients should be counselled on what to expect regarding bleeding pattern changes Women should be reassured that bleeding with dienogest 2 mg is not a sign of a lack of efficacy or recurrence of disease Two distinct types of bleeding irregularities may occur during dienogest 2 mg treatment: initial bleeding during the first few months, and bleeding/spotting with longer-term use Initial bleeding can be consistent and typically lasts for 8–10 days. A regimen involving treatment with a releasing hormone followed by long-term dienogest therapy may reduce initial irregular bleeding77. Furthermore, initiation of dienogest 2 mg at the onset of menses may also decrease initial bleeding Bleeding that occurs during long-term treatment is typically spotting.
- The occurrence of abnormal uterine bleeding may require further investigation, such as by ultrasound examination. Persistence of abnormal uterine bleeding should prompt further investigations for other uterine pathologies beyond endometriosis.
- Recording sexual history and screening for sexually transmitted infections may be advised
- ORAL CONTRACEPTIVE PILLS
- LIFESTYLE MODIFICATION
- ANTIFIBRINOLYTIC AGENTS
- GNRH AGONISTS
- DIENOGEST
All the above drugs have been tried with no permanent cure. They have various side effects like stoppage of menses for the period for which they are given, flushes, bone pain, weight gain, only temporarily relief and irregular bleeding pv.It is just like delaying the inevitable. The current opinion is that definitive treatment is only by surgery and that too by a skilled surgeon who has experience, enough cases of endometriosis under his belt and has a sound knowledge of the disease. It is often said that the first surgeon doing the surgery has the best chance of removing the whole disease. Subsequent or re do surgeries become more difficult and challenging.
That is the only reason why we have come with the concept of the ODISHA CENTRE FOR L.I.F.E ( LAPAROSCOPY, INFERTILITY, FIBROIDS AND ENDOMETRIOSIS) to provide a one stop solution to all our patients in the best and complete way possible. The purpose is to treat with methods and drugs at par with international standards, minimise symptoms, optimise fertility, and prevent recurrence. The surgery is done by DR G S S MOHAPATRA, trained at numerous places like France , Germany, Italy for laparoscopy in endometriosis and the technology used in the form of camera system and the gadgets and instruments used are the most advanced and world class.
The most recent studies have shown that endometriosis recurs at a rate of 20% to 40% within five years following conservative surgery, . The use of oral contraceptive, other suppressive hormonal therapy, or progesterone intra uterine device (IUD) after surgery has been shown to reduce the recurrence of pain symptoms but does not remove the disease. Hence the wise option is to go for surgery with a motive to all diseased tissue as much as possible to alleviate symptoms, remove disease and prevent recurrence.
With more advanced endometriosis (Stages 3 or 4), surgery can help restore your normal pelvic anatomy to allow the ovaries and fallopian tubes to work better. Surgery to remove large endometriomas may also improve fertility rates. There have been many studies in this regard with a few suggesting surgery helps while others have suggested just the opposite. In our experience, FERTILITY ENHANCING SURGERIES play a pivotal role in early stages of endometriosis with infertility and in the later part an adhesiolysis helps in egg retrieval during the procedure of IVF.
Deep infiltrating endometriosis (DIE) is a particular form of endometriosis that penetrates >5 mm under the peritoneal surface (Koninckx and Martin, 1994). These lesions are considered very active and are strongly associated with severe pelvic pain.It is stage III or stage IV of endometriosis .It involves organs within the pelvic cavity and can plaster the ovaries, rectum, uterusto each other and can even lead to a drastic condition called as FROZEN PELVIS.
- Specific MRI or TVUS protocols are highly accurate in making a nonsurgical diagnosis of deep infiltrating endometriosis (DIE).
- The combination of compelling clinical signs and symptoms and absence of imaging findings for DIE can be used to make a presumptive nonsurgical diagnosis of endometriosis.
- Empiric medical therapy may provide pain relief.
- Conservative treatment, including observation alone, may be considered in asymptomatic patients with DIE and in those with minimal pain.
- Before surgery, it is imperative to know lesion size, depth, circumferential bowel involvement, and location to optimize surgical outcomes.
Endometrioma is one of the most frequent adnexal masses in the premenopausal population, but the recommended treatment is still a subject of debate. Medical therapy is inefficient and can not be recommended in the management of ovarian endometriomas. The general consensus is that ovarian endometriomas larger than 4 cm should be removed, both to reduce pain and to improve spontaneous conception rates. The removal of ovarian endometriomas can be difficult, as the capsule is often densely adherent. While the surgical treatment of choice is surgical laparoscopy, for conservative treatment, the preferred method is cystectomy. We only remove the cyst wall and leave behind the ovary. Hence the ovarian function is preserved. The procedure is done in young unmarried females, in women who are desirous of fertility, who are young, preferably below the age of forty.
A skilled surgeon who understands the needs of the patient is a must because the AMH ( indicator of ovarian reserve) should not be going down drastically after the surgery. The surgeon should be conservative towards fertility and radical towards the disease.
- https://www.youtube.com/watch?v=yfiWD5iWdYI Laparoscopic chocolate cystectomy by DR G S S MOHAPATRA
- https://www.youtube.com/watch?v=FvnEFRMmxBo Chocolate cystectomy by DR G S S MOHAPATRA
HOSPITAL
- ANKURA HOSPITAL, BHUBANESWAR
- 9937776329
- NURTURE MOTHER & CHILD clinic GA 190 Gayatri Vihar, Nandankanan Road, Patia Chowk, Next to STYLIVE Furnishings, Jasodha Homes, Bhubaneswar, Odisha – 751024
- 9776822222
drgssmp@gmail.com
NURTUER Mother and Child Clinic. Patia
ANKURA HOSPITAL, BHUBANESWAR












